Search
Otitis media with effusion (OME) affects hearing, speech development, and quality of life (QoL) in children. The 'Blow, Breathe, Cough' (BBC) intervention promotes nasal, respiratory, and middle ear clearance through nose blowing, deep breathing, coughing, and hand hygiene. It shows promise in resolving OME but lacks randomized-controlled trial (RCT) evaluation. This paper presents a RCT protocol evaluating BBC's effect on OME resolution, hearing, speech, and QoL in children aged two to seven years.
Otitis media (OM), or middle ear infection, is one of the most common childhood illnesses globally. In Australia, OM remains a leading cause of antibiotic prescriptions in children, despite growing awareness of antimicrobial resistance (AMR) and the need for stewardship. Preventing OM not only reduces the burden of disease but also plays a critical role in curbing unnecessary antibiotic use and slowing the rise of AMR.

Two projects led by The Kids Research Institute Australia have been awarded more than $2.5 million to fund innovative ideas focused, respectively, on combating persistent ear infections and investigating how dangerous fungi invade the bodies of immunocompromised people.
Small volume assays are required for large-scale research studies and in particular paediatric trials, where multiple measures are required from a single sample. Fluorescent bead-based technology (Bioplex/Luminex) allows high through-put and simultaneous quantification of multiple analytes in a single test. This technology uses sets of microspheres, each with a unique spectral address that can be coated with a different antigen of interest.
A birth acellular pertussis vaccine may be a valuable alternative for immunity against infant pertussis when a pregnancy pertussis vaccine has not been administered. We assessed whether a birth dose may impair immunoglobulin G (IgG) responses to childhood pertussis boosters.
We assessed the impact of maternally derived pertussis antibodies on infant responses to a 2 + 1 vaccine schedule (6 weeks, 12 weeks, and 12 months). Infants with baseline antibodies showed lower IgG responses following the primary vaccination series, but this did not impair booster responses at 4 years of age.

Children at risk of potentially life-threatening Strep A infections no longer have to wait five days for timely treatment, thanks to a The Kids Research Institute Australia study conducted in the remote Kimberley region of Western Australia.

Findings from The Kids Research Institute Australia’s ‘Ear Explorers’ real-life research project undertaken as part of the 2019 Telethon weekend, found short videos were more helpful than photos when making a diagnosis.
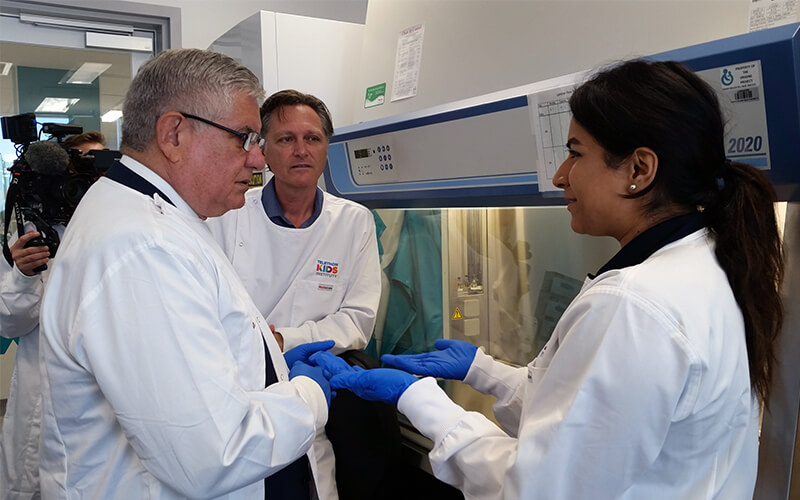
A vaccine to prevent rheumatic heart disease (RHD) and other life-threatening conditions caused by the common Strep A bacteria is a step closer thanks to funding announced by Minister for Indigenous Health, Hon Ken Wyatt AM, MP, in Perth today.

In a WA first, researchers from The Kids Research Institute Australia have shown that Aboriginal babies are 22.5 times more likely to be treated for skin infections than non-Aboriginal babies.
